Remote monitoring
The remote monitoring-enabled delivery of care programme is a collaborative, multi-disciplinary project delivered by partners across health and social care, including: The Programme Board, NHS Coventry and Warwickshire CCG, NHS Coventry and Warwickshire Partnership Trust, NHS George Eliot Hospital, NHS Integrated Care Community, NHS South Warwickshire Foundation Trust, Warwickshire County Council, North Warwickshire Primary Care Networks, Graphnet and Arden and Gem CSU.
The pilot started at the Hazelwood practice in Coleshill, where COPD patients who had had one hospital admission in 12 months or had used two ‘rescue packs’ were selected. Rescue packs contain steroids and medication for people who are unwell with COPD. Feedback from these patients demonstrates that they have been benefiting from improved access to clinicians and reduced anxiety ever since. There are currently approximately 170 active COPD patients on the scheme.
How does the COPD remote monitoring scheme work?
Victoria Foster, Clinical Practitioner for Docobo remote monitoring in a Box and Care Homes at South Warwickshire NHS Foundation Trust, explains:
The patients we selected for the initial pilot were those who were often anxious about their condition. As COPD is a respiratory disease and breathlessness is one of main effects, many patients can become anxious as they are not able to get a full breath.
These patients were given a ‘Docobo in a box’ pack which includes a Nokia 10 phone, a pulse oximeter, a thermometer and a blood pressure monitor. Patients were asked to record observations such as temperature, blood pressure, and oxygen saturation levels by midday on a daily basis. They enter the information onto the Nokia 10 phone, and this clinical information is then sent to the dedicated call centre. If something is not quite right, the system will flag up an alert which will be picked up by a nurse in the call centre. The alert is then triaged and if nurses think the patient need a visit, they will organise this.
What are the benefits to patients and teams?
Victoria explains:
It’s great that our COPD patients have access to nurses. They review the alerts, and even if there is not a major problem, they will telephone the patient and reassure them and check if they need a visit. If the nurse feels a visit is necessary, it will go through to an urgent response team or come through to myself. If it’s a complex but not urgent request, it will come through and be triaged by the ICC team.
Those patients that are alerting quite frequently, or who are anxious as to how their COPD is progressing, are put through to me. I then work with them and visit them to see what we can do to improve this, for example, teaching breathing techniques etc. The feedback we have received has been so positive, people have fed back that – using this system – they feel much less anxious, more supported in own home, more confident and able to carry out daily activities.
Victoria also works alongside a respiratory specialist nurse, and when an alert comes in that he should deal with, he goes out to his Multidisciplinary team and COPD consultant to investigate. As COPD can sometimes progress to heart failure, Victoria also works with a heart failure nurse.
How does remote monitoring work?
Remote monitoring enables users to update personal healthcare data using different kinds of question sets, which are then recorded and submitted to clinicians using a secure web interface. This pilot involved a special COPD question set that was developed by the team. Remote monitoring uses the DOC@HOME platform to do the following.
- COPD patients daily record their vital signs and symptoms onto the Nokia 10 (using thermometer, blood pressure monitor, pulse oximeter etc).
- They are asked a few specific question sets – i.e. how is your breathing etc.
- Nurses triage the alert and will respond within 2 hours – either with a GP or nurse call out or a telephone call.
- The patient is reassured that their symptoms are being reviewed and are comforted by this.
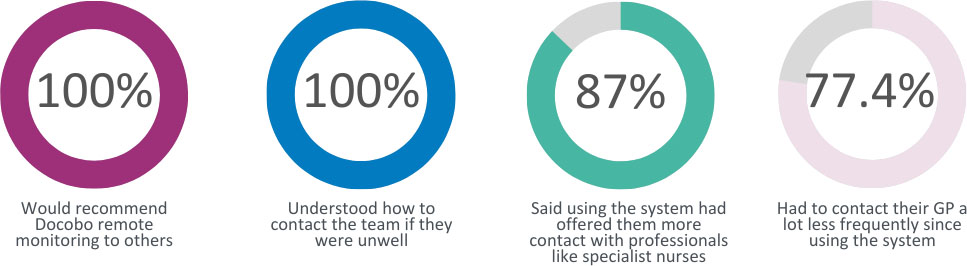
Excellent Patient Feedback
The nurses that contact me have been brilliant and really supportive. I feel more confident.
I struggled to use the system initially but now get on really well with it.
Victoria concludes:
I’m so pleased with the results from this pilot, it’s great! With new patients, once the parameters are set – they tick along and are monitored 7 days a week – which I think is fabulous. I have many examples of how this is working brilliantly. I spotted a patient whose blood pressure readings were coming in high every day. We started them on medication to reduce the readings, which worked really well. This could have prevented a heart attack or stroke, essentially saving a life and preventing a catastrophic event.









